Introduction
Prone ventilation, or placing patients face-down, has emerged as a pivotal intervention in managing Acute Respiratory Distress Syndrome (ARDS). This technique has garnered significant attention between 2020 and 2024, especially during the COVID-19 pandemic, highlighting its relevance for respiratory therapists and physicians.
Understanding ARDS
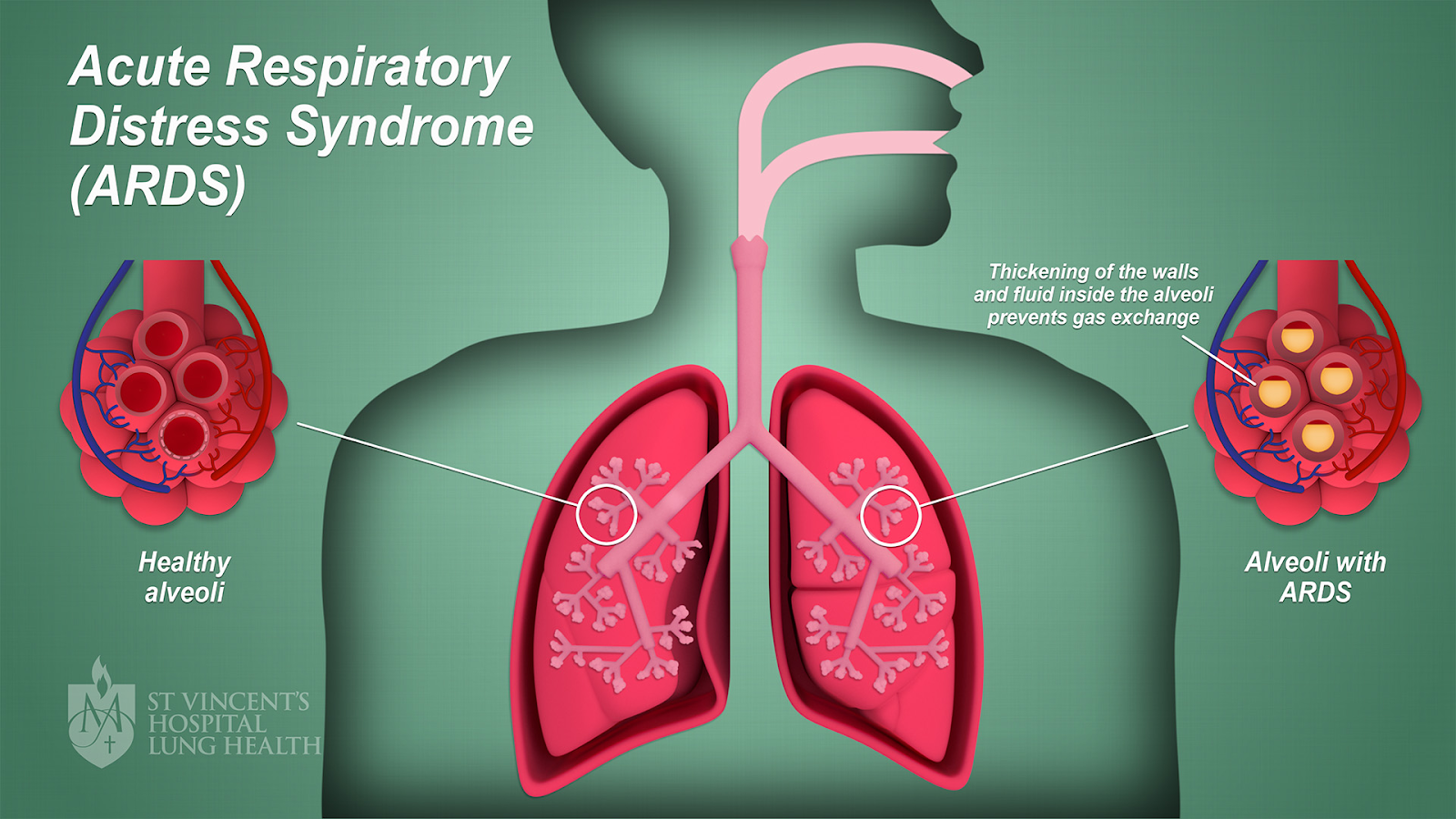
ARDS is a severe lung condition characterized by rapid-onset inflammation and increased pulmonary vascular permeability, leading to hypoxemia and respiratory failure. Common causes include pneumonia, sepsis, trauma, and inhalation injuries. The hallmark of ARDS is the accumulation of fluid in the alveoli, resulting in impaired gas exchange and decreased lung compliance.
The Berlin Definition
The Rationale Behind Prone Ventilation
The supine position in mechanically ventilated patients can exacerbate lung injury due to gravitational forces, leading to atelectasis in dorsal lung regions and overdistension in ventral areas. Prone positioning redistributes these forces, promoting more uniform lung aeration and perfusion. This results in improved oxygenation and reduced ventilator-induced lung injury (VILI).
Physiological Benefits of Prone Positioning
1. Improved Oxygenation: Prone positioning enhances ventilation-perfusion matching by recruiting posterior lung regions, leading to better oxygenation. Studies have shown significant improvements in the PaO₂/FiO₂ ratio with prone positioning.
2. Reduction in VILI: By promoting more homogeneous lung inflation, prone positioning decreases the risk of VILI, a critical consideration in ARDS management.
3. Enhanced Secretion Clearance: The prone position facilitates mucus drainage, reducing the risk of ventilator-associated pneumonia.
Understanding West Zones
The lungs are divided into three zones based on the relationship between alveolar pressure (PA), arterial pressure (Pa), and venous pressure (Pv):
Zone 1 (Dead Space): PA > Pa > Pv
- Minimal or no blood flow due to high alveolar pressure compressing capillaries.
- Typically occurs in the apex of the lungs in the upright position.
Zone 2 (Waterfall Zone): Pa > PA > Pv
- Blood flow depends on the difference between arterial and alveolar pressures.
- Middle regions of the lungs in upright patients.
Zone 3 (Perfusion Zone): Pa > Pv > PA
- Continuous blood flow occurs as capillaries are fully distended.
- Typically found in the dependent regions of the lungs (posterior in supine, anterior in prone).
image credit
West Zones in Prone Ventilation
When a patient is in the prone position, the distribution of West Zones shifts due to the reorientation of the lung and chest wall relative to gravity:
Supine Position:
- The dorsal (posterior) lung regions, typically Zone 3, are compressed by the heart and abdominal contents.
- Ventilation predominantly occurs in non-dependent ventral (anterior) regions, leading to ventilation-perfusion (V/Q) mismatch.
Prone Position:
- Dorsal regions, previously compressed, now expand as gravitational and compressive forces redistribute.
- Ventilation increases in these dorsal regions, which often correspond to areas with better perfusion (Zone 3).
- This leads to improved V/Q matching and oxygenation
Clinical Evidence Supporting Prone Ventilation (2020-2024)
Recent studies have reinforced the efficacy of prone ventilation in ARDS patients:
Mortality Reduction: Prone ventilation has been linked to a reduction in mortality among ARDS patients. Research indicates that employing prone positioning for at least 16 hours daily can significantly decrease 90-day mortality without substantial adverse effects.
Synergistic Effects with Low Tidal Volume Ventilation: When combined with low tidal volume ventilation, prone positioning may exhibit synergistic lung-protective effects. The survival advantage of the prone position seems contingent on the concurrent use of low tidal volumes.
Feasibility and Safety: Extended prone position ventilation has been deemed feasible and relatively safe for treating critically ill patients with ARDS, including those with COVID-19-related ARDS. This suggests potential implications for a broader acceptance of prone ventilation in ARDS management.
Implementation Strategies for Respiratory Therapists and Physicians
1. Patient Selection: Not all ARDS patients are ideal candidates for prone ventilation. Consider factors such as hemodynamic stability, absence of contraindications (e.g., spinal injuries), and the severity of hypoxemia.
2. Timing and Duration: Early initiation of prone positioning, especially within the first 48 hours of ARDS diagnosis, is associated with better outcomes. A cumulative duration of more than 32 hours during the first 48 hours of ICU admission has been linked to improved outcomes.
3. Team Coordination: Prone positioning requires a coordinated multidisciplinary approach to ensure patient safety and minimize complications. Regular training and simulation exercises can enhance team efficiency.
4. Monitoring and Assessment: Continuous monitoring of oxygenation parameters, hemodynamics, and potential pressure points is crucial. Adjustments should be made based on the patient's response to prone positioning.
Challenges and Considerations
While prone ventilation offers significant benefits, it also presents challenges:
Complications: Potential complications include pressure injuries, accidental extubation, and facial edema. Implementing evidence-based strategies to prevent these complications is crucial.
Resource Intensiveness: Prone positioning is labor-intensive and requires adequate staffing and equipment. Ensuring the availability of trained personnel and appropriate equipment is essential for successful implementation.
Patient Tolerance: Not all patients may tolerate prone positioning. Regular assessment and prompt management of any adverse effects are necessary to ensure patient comfort and safety.
Conclusion
Prone ventilation has solidified its role as a cornerstone in the management of ARDS, offering improved oxygenation and survival benefits. The period from 2020 to 2024 has provided robust evidence supporting its efficacy, particularly during the challenges posed by the COVID-19 pandemic. For respiratory therapists and physicians, understanding the nuances of prone positioning, from patient selection to implementation and monitoring, is essential. By embracing this technique, healthcare professionals can enhance patient outcomes in ARDS, turning the tide in the battle against this formidable condition.




.jpeg)

No comments:
Post a Comment