Unraveling Mpox: A Modern Challenge in Global Health
Emerging disease outbreaks have frequently taken center stage in the recent problems facing the global health landscape. Mpox, formerly known as monkeypox, is one such disease. Despite being around for decades, outbreaks outside of its natural endemic regions have made it more significant in terms of public health. The purpose of this blog is to provide information about Mpox, its effects on human health, and the steps we can take to safeguard our communities and ourselves.
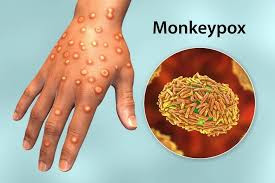
The Mpox virus, which relates to the Orthopoxvirus genus, is the cause of the viral infection known as mpox. Although Mpox is typically less severe, it is closely related to the virus that causes smallpox. Although rodents are probably the disease's natural hosts, it was initially discovered in 1958 in study monkeys, hence its original name. The Democratic Republic of the Congo reported the first human case in 1970.
Symptoms and Transmission
Flu-like symptoms like fever, chills, and muscular aches are the first signs of mpox. A rash that usually starts on the face and spreads to other areas of the body follows. After going through several phases, the rash finally forms scabs and falls off.
Close contact with an infected person or animal, as well as contaminated bedding or other materials, can spread the infection. Human-to-human transmission mostly occurs by bodily fluids, direct contact with lesions, or respiration droplets. For prevention, it is essential to comprehend these ways of transmission.
Why Mpox Matters Today
For many years, Mpox was limited to specific areas in Central and West Africa. However, recent outbreaks in countries where disease is not endemic caused around the world. Factors such as increased international trips, climatic change, and low smallpox vaccination coverage—which provides some cross-protection against Mpox—may all contribute to its spread.
The 2022 outbreak, for example, included patients from Europe, North America, and other countries, indicating how linked our globe has grown. The necessity of strong surveillance systems and quick response plans was highlighted by this outbreak.
Prevention and Protection
Vaccination: It has been demonstrated that the smallpox vaccine is effective against Mpox. Vaccination initiatives can aid in controlling the spread of an outbreak.
Hygiene Practices: It's crucial to wash your hands frequently and keep your distance from infected people or animals.
Community Engagement: Encouraging open communication and combating disinformation can help communities act responsibly.
Healthcare Access: Timely diagnosis, treatment, and containment are ensured by strengthening healthcare systems.
The Human Angle
Beyond the science, it is critical to understand the human stories around Mpox. Outbreaks frequently disproportionately impact underprivileged areas with limited access to healthcare. The stigma associated with the illness can make it more difficult for people to report cases and seek treatment, which will accelerate its spread. Compassionate communication and inclusive policy are critical for tackling these issues.
Looking Ahead
As the globe continues to struggle with Mpox, collaboration is our most effective tool. Governments, healthcare professionals, researchers, and individuals must collaborate to create robust systems capable of combating not only Mpox, but also other emerging infectious diseases.
.jpeg)
.jpeg)

No comments:
Post a Comment